Have you Heard of Histamine Intolerance?
Histamine Intolerance wasn’t something that was on my radar over the last few years in the health and wellness space. My focus was usually on autoimmunity, blood sugar regulation, and gut health. However, all those things also apply to histamine intolerance, and many of the foods I don’t eat (i.e. tomatoes) are high in histamine. When my friend and colleague Dr. Campbell published her 2nd book, the 4-Phase Histamine Reset Plan, I was so intrigued by this new (to me) facet of healing through food.

I now work with Dr. Campbell in her virtual Functional Medicine Clinic and help her patients dive into healing protocols, including a low histamine plan. Dr. Becky Campbell was gracious enough to share this insightful article on how histamines can be contributing to your symptoms, even on a healthy diet!

Why Your New Diet May Be Making You Sick | by Dr. Becky Campbell
Did you just recently start a Whole 30, Paleo, or Keto diet, only to find that now you’re feeling worse than you did before?! As it turns out, many of these “healthy” foods that are integral components of many of these diets are also very high in extrinsic histamines, which can cause a problem for someone with histamine intolerance. But what exactly does this mean?
It is important to note that histamine is an integral and required part of a healthy immune system – the goal is never to rid your body of histamines entirely. It is an important neurotransmitter and it creates necessary inflammation during any sort of immune system response, whether it’s related to injury, disease, or other foreign matter. Histamine levels of 0.3 to 1.0 nanograms per milliliter (ng/mL) in plasma are considered to be normal (1).
Histamine, among many other chemical inflammatory mediators, is released from mast cells. Mast cells are located in connective tissue, like the lining of the gut, skin and other sites in the body. These cells play a very important role in helping defend these tissues from disease by releasing chemical “alarms”, like histamine, to areas of the body where they are needed.
For example, if someone is extremely “allergic” to peanuts, the slightest taste can trigger an immense histamine response. This response results in systemic inflammatory signals – to your nose, throat, mouth, gut, skin, and lungs. This “allergic reaction” caused by histamine is likely why this inflammatory chemical gets such a bad reputation.
Like anything, too much of a good thing is a problem, and when we accumulate too many histamines and our bodies can’t break them down fast enough, that’s when we begin to see symptoms of histamine intolerance. We all technically have some degree of “histamine intolerance,” but it is important to remember that it is a dynamic process, affected by allergic reactions, diminished genetic ability to clear histamine (decreased Diamine oxidase AKA DAO, the enzyme that breaks down histamine, production), compromised gut health (leaky gut, gut infections, irritable bowel syndrome), lifestyle (stress and ingestion of substances that block DAO, like NSAIDS and alcohol), and food that is high in histamines (2,3). Consider this quote from Chris Kresser:
Histamine intolerance is unlike other food allergies or sensitivities in that the response is cumulative, not immediate. Imagine it like a cup of water. When the cup is very full (high amounts of histamine in the diet), even a drop of additional water will cause the cup to overflow (symptoms activated). But when the cup is less full, it would take more water (histamine) to cause a response. This makes histamine intolerance tricky to recognize.

The Histamine Bucket
Think of your tolerance to histamine like a bucket. When you’re stressed at work, taking NSAIDs (ie. Advil) to get rid of the headache you have to make it through the day, not sleeping well, and too tired to cook yourself a decent meal, you are more at risk for your “bucket” to overflow, resulting in the “allergic reaction-type” symptoms that you would expect (3). We would label this as a histamine intolerance – you are not clearing the histamine in your body fast enough – but that doesn’t mean you’ll have these symptoms forever! I really like how this phenomenon is described by Dr. Janice Joneja:
A person with histamine intolerance will typically experience a constant fluctuation in the signs and symptoms of histamine excess in response to changing conditions. For example, when a person is experiencing an allergy to airborne allergens such as seasonal pollens, the histamine released in the allergic response alone might put them into the symptom range. In such a case, avoiding histamine-associated foods will no longer relieve their symptoms because their total level of histamine will remain above their limit of tolerance. This explains the observation that during their “pollen allergy season” many people find themselves reacting to foods (usually histamine-rich foods) that they could normally eat with impunity (1).
Role of MCAS in Histamine Intolerance
As mentioned by Kresser and Joneja, histamine intolerance is not so much of a diagnosis as it is a collection of a bunch of symptoms. It is now believed that Mast Cell Activation Disorder (MCAD) is a more accurate depiction of what is happening in patients who have been diagnosed with “histamine intolerance.” Mast cells are located in most tissues of the human body, especially in connective tissue, skin, and the digestive, cardiovascular, nervous, and reproductive systems. When the body is exposed to perceived threats, mast cells quickly secrete chemicals, like histamine, interleukins, prostaglandins, cytokines, and other various chemicals stored in cells to address the issue. Both local and systemic effects are the result, such as increased permeability of blood vessels, which will cause increased inflammation and swelling, smooth muscle contractions that may lead to heart palpitations and stomach cramps, and increased mucous production that will cause increased sneezing and coughing. We initially only thought that mast cells were related to allergies, but now we know that they likely play a much larger role in over-activation of the immune system as well as the development of other autoimmune disorders, especially though involving antibodies, probably related to the presence of more environmental toxins and chemicals. MCAS has been linked to the development of allergies, asthma, autism, autoimmune diseases (Hashimoto’s thyroiditis, lupus, multiple sclerosis, rheumatoid arthritis), eczema, Celiac disease, chronic fatigue syndrome, chronic inflammatory response syndrome (CIRS), fibromyalgia, food allergies, GERD, infertility, IBS, migraines, anxiety/depression, and postural orthostatic tachycardia syndrome (POTS) (4).
Overactive mast cells can cause a variety of symptoms including skin rashes, swelling, flushed skin, itching, abdominal pain, nausea/vomiting, diarrhea, wheezing/shortness of breath, heart palpitations, anxiety, headaches, brain fog, low blood pressure, and fatigue.
Managing MCAS and Histamine Intolerance with Food
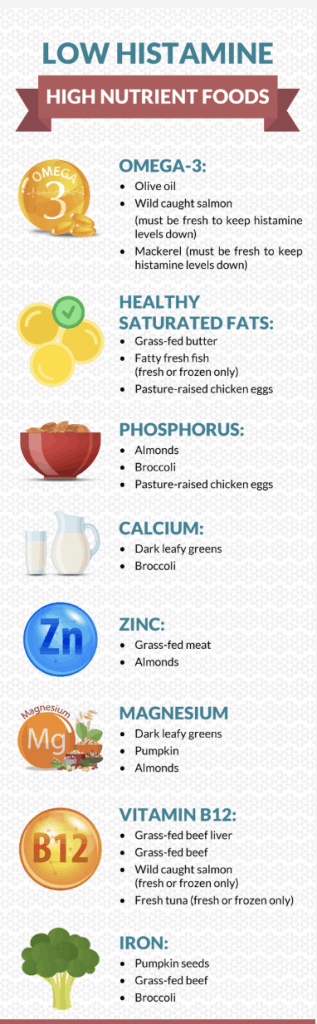
The good news is there are many foods that do act as natural antihistamines and mast cell stabilizers! Looking for foods that contain ascorbic acid, quercetin, vitamin B6, omega-3 fatty acids, and riboflavin can help reduce the amount of histamine you are producing.4
Sometimes, at least while you are experiencing a flare-up of your MCAS, it may be helpful to eliminate foods known to contain high histamine content. Foods may naturally have more histamine content, while other foods accumulate more histamine as they age. Please notice that many of the foods listed below are primary staples in any Whole 30, Paleo, or keto diet! Histamine-rich foods include:
- Fermented alcoholic beverages, like wine, champagne, and beer
- Fermented foods like sauerkraut, vinegar, soy sauce, kefir, yogurt, kombucha (don’t shoot the messenger!)
- Foods high in vinegar like pickles, mayonnaise, olives
- Cured meats like bacon, salami, pepperoni, deli meats, hot dogs
- Soured foods like sour cream, sour milk, buttermilk
- Dried and citrus fruits
- Aged cheeses
- Nuts
- Vegetables like avocados, eggplant, spinach, tomatoes
- Any smoked fish and certain fish species like mackerel, mahi-mahi, tuna, anchovies, sardines
- Any processed foods (preservatives contain high amounts of histamines).5
It is important to remember that ingesting histamine is not the only cause for an increase in histamine in your body. Once an immune response is complete, there need to be enzymes to break down the histamine and other chemical mediators that were released. Diamine oxidase is the enzyme that is primarily responsible for breaking down histamines. Once broken down, they are excreted through your urine via the kidneys. Usually, sufficient DAO in the small intestines means that the histamine you ingest is broken down before it causes a problem. However, if you are DAO deficient, histamine isn’t being broken down as readily, resulting in an increase in histamine levels. If you experience this increase in histamine for a prolonged period of time, the result is Mast Cell Activation Disorder, chronic inflammatory, and histamine sensitivity.

Supplement Support for Histamine Intolerance
I recommend to patients a supplement called histo-relief, which includes quercetin (a mast cell stabilizer) as one of its primary ingredients. This supplement supports immune function, as well as the body’s response to food and environmental factors. I have seen many of my patients become a lot more tolerant to food when adding this supplement to their daily regimen. Certain probiotics also limit histamine production – look for items with Lactobacillus rhamnosus and bifidobacter. I like ProBiota HistaminX by Seeking Health.
I think it is helpful for people to realize that they are not alone – histamine intolerance is not something that Western medicine typically recognizes. It is important to recognize these symptoms don’t have to be forever and are also not just about what you eat. Yes, you may just have started on a diet where you are eating a ton of new foods, many of them very histamine-rich, but you also have to take into consideration your environment? What season is it? Are you stressed? Have you been sick or been on antibiotics? All of these things can overflow your histamine “bucket” and make it so even if you are watching your foods, it may not be enough to control your histamine response if your “bucket” is also almost overflowing.
Maybe instead of your high histamine diet, you try a low histamine reset diet while working on the underlying causes before reintroducing histamine-rich foods. Maybe you add in some yoga and meditation to help control your stress levels. Figure out why your histamine may be elevated and then make the changes required. If you’ve already tried this and hit a roadblock, please feel free to set up a consultation with me. I would love to help you get a grip on your symptoms and take your life back!
Bye, Bye avocado toast….at least for now!





Susan J says
Thank you for this very helpful article. I have alpha gal tick syndrome, which causes severe allergy to mammal and has caused many of us to have high histamine and MCAS problems. This helps explain the histamine bucket process. I plan on sharing your article with my AG group.
Tony says
Thank you to provide such a good information regarding histamine intolerance. This will help to keep myself save.
Amy says
Thanks for this article! It’s interesting that you listed salmon and beef under low histamine foods – I was under the impression that salmon had to be fresh-off-the-boat fresh which seems like a difficult task, and that beef is almost always aged so is higher in histamines as well. Is this incorrect information? I’ve been noticing that too much beef can be triggering for me.
And is Dr. Campbell’s book a good resource for someone already stuck on the AIP? I’ve been in flares pretty consistently since last July and don’t know how to do reintro’s when I’m already having some symptoms and many non-AIP foods make symptoms worse.
Cristina Curp, FNTP says
Yes, salmon does have to be very fresh, as noted in the graphic. Beef too, all meat has to be fresh or frozen to keep histamine levels down. No leftovers, all animal proteins need to be thawed cooked and eaten or frozen again. The book has a lot of information on histamine, the recipes arent very AIP friendly. There could be something going on with your gut that diet alone is not targeting.
Christin J Slyngman says
wow! This article is REALLY helpful! I’ve been trying to get to the root of my Interstitial Cystitis, migraines, and constant mucus/cough issues…she suggested it might be a histamine issue after my allergy tests came negative, and after reading this I’m beginning to connect the dots with my symptoms and my eating habits…thank you so much for posting this!
Amy says
Thank you for shedding light on Histamine Intolerance and MCAD! It has been so difficult to find anyone in the Paleo world who gets this!!! I was diagnosed with MCAD and Hashimoto’s Thyrioditis as a result. I have been extremely fortunate to have found an MD in my area who specializes in MCAD and Autoimmune Diseases. While she now has me on the right path to healing (which most days feels like full time job, btw!) after extensive lab work and supplementation, I still feel like I’m on my own in the kitchen! I have scoured the internet for recipes, meal plans, cookbooks that are AIP, grain-free (I’m also Celiac), and low histamine! THEY SIMPLY DON’T EXIST for people like me!!! I’ve instead had to tweak and reinvent my already paleo, keto, whole 30 recipes to get any kind of food in me. You would be helping a vast community if you could create some sort of cookbook with detailed meal plans, recipes with modifications (such as low oxalate, fodmap, sugar-free, etc), and information about MCAS! The word needs to get out more and help is much needed! I hope that you will consider taking on this challenge! 🙂 I guarantee you, it would help many who are suffering like me. Thank you, even for just bringing up this topic! This line alone, “but that doesn’t mean you’ll have these symptoms forever!” gave me so much hope!!!
Cristina says
Hi AMy! Dr. Campbell’s book, The 4 Phase Histamine Reset Plan does have grain free, paleo Histamine recipes! You’re going to love it
Amy says
Thank you, Cristina! I ordered Dr. Campbell’s book and hope it will help. Thanks again for raising awareness in MCAS!
Tonya Harpe says
Thank you so much. I got more out of this article than I’ve ever gotten out of the two major allergy/immunology clinics I see (besides the flood of antihistamines & mast cell stabilizing drugs they prescribe me). I keep seeing allergists who want to send me to another specialist, like an ENT doctor for migraines or inner ear problems/dizziness, rather than acknowledge HIT. There’s only 1 true doc in my whole state, or maybe even further out, who tests for HIT. I’ve been on a 7 month long waiting list just to get a HIT test & now this doc will no longer do future HIT testing or see new patients, so I just barely made it on his schedule to get HIT testing these next weeks, but he will NOT be my immunologist/internist which I really need. It’s terrible how few practitioners in the states recognize this devastating problem, much less link HIT to MCAS, but I’ve been telling my doctors to pay attention to the symptoms because they may save their other patient’s lives. For one thing, when your doctor routinely prescribes meds that overflow your histamine bucket, it can make you extremely ill & you won’t understand why you’re getting worse instead of better. Then there is the postop pain flareup. Any type of minor dental surgery flares me so badly. Also most days I fight bone & muscle pains, all “unseen” symptoms, so they’re ignored by my doctors. What’s worse, the NSAID’s I’m forced to take for these awful pains only fills my H bucket in the end, so this too will sicken me. If only this problem could be treated by diet & diet alone, well I wouldn’t be leaving this long drawn out comment. Good luck finding the correct doctor. It’s a lot easier in Europe, but incredibly hard in the US.
Margaret J Wright Percy says
I am very histamine intolerant, and have used the DAO food supplement and that is the only thing that helped me, so I’m looking for another container of DAO supplement, it is available in Spain but not in the USA and the price can be exorbitant…maggie my intolerance comes with itchiness all over my skin.
Pat Gl says
WOW! Was your article timely! I experienced itching for 2 days last week that seemed to be like hives, except there weren’t any bumps. For some reason, my mind went to 2 instances where I ate avocados — the first day on a sandwich, the second guacamole with crackers for a quick dinner. (I don’t usually eat avocados.) The article seems to explain what I was experiencing! I will have to look more at what I am eating.
Barbara Ruccione says
Excellent article. I have migraines from histamine intolerance. Everything you said here us correct except the ascorbic acid. That gives me intense migraines.
Cristina says
I’m glad you enjoyed the article by Dr. Campbell. As for the ascorbic acid it helps some people, not everyone is the same 🙂
Natalie says
What an eye opener! I’ve never heard of this but does give me a lot to think about and take into consideration. Thank you for sharing!!
Arlene Estrella says
This was a great article. I have been aware of histamine intolerance because I suffer from it and I had to learn this on my own. This is nice and simple.